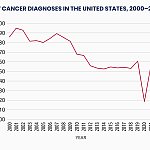
Rising measles cases in the United States underscore the impact of low childhood vaccination rates, which have declined in recent years.
As measles cases approach
What began as a small outbreak in a Mennonite community in West Texas in January spread to at least 30 U.S. jurisdictions by the end of April. According to the Centers for Disease Control and Prevention (CDC),
Measles was declared eliminated at the turn of the century. Now, researchers warn the disease could make a strong comeback in the next 25 years, with up to 51 million new illnesses if vaccination rates fall below 50%.
The projection, published April 24 in
Measles is
“Measles is in the midst of a substantial resurgence in the United States at the present time,” said William Schaffner, MD, professor of preventive medicine and infectious diseases in the Department of Health Policy at Vanderbilt University Medical Center in Nashville.
“Before we had the vaccine, measles killed
Healthline spoke with Schaffner to find out how concerned people should be about measles returning to endemic status in the United States and what can be done to help reverse current trends.
This interview has been edited and condensed for clarity and length.
Schaffner: I think it’s a worst-case scenario. It’s possible, but it won’t get that bad.
That said, there are many communities in which vaccination rates have drifted down to 90% or even lower. In some communities, they’re very low, and we could continue to have outbreaks in those communities.
As we see in West Texas, this is now a very prolonged, even accelerating outbreak because there has been a very large community that is under-vaccinated.
So yes, we could lose our elimination status, but I don’t think it will be as bad as this worst-case scenario suggests. That is not to say I don’t think it’s awful — it is definitely alarming.
Schaffner: What we are seeing now will be expanded, namely clusters of measles around the country, as the virus is reintroduced into those communities where there is a very low vaccination rate, and then you’ll get bursts of measles in that community.
Fortunately, previous measles infection and vaccination provide very secure protection.
Relatively few people who’ve been previously vaccinated will become infected. So, we will have barriers of previously vaccinated folks and older people who were infected with the virus, which will confine measles to those under-vaccinated populations.
Schaffner: I hesitate to say that we would have to learn to live with it, because that’s a profoundly sad prospect.
The short answer is yes, and it will continue to occur in bursts because there will be many communities in the United States where vaccination levels will remain very, very high, well above 90%. That’s because those are communities where parents will conform to ‘no shots, no school’ policies, and you will get very high vaccination levels, as we have had in the past.
However, there are communities sometimes defined by a social phenomenon or a religious affiliation, for example, where vaccination rates are very low in that localized community.
One of the consequences of having these pockets of susceptible children is that when the virus enters those populations, the children will tend to be older than they were in the bad old days when they got measles, because they’ve been protected. They’ve had to wait for the virus to be introduced.
And you’ll have many more adolescents, for example, who’ve never experienced measles.
Complications occur at any age, but the older you are when you acquire measles, for example, if you’re a teenager, as many of these children are now who are acquiring infection in West Texas, the more likely you are to develop one of the complications.
Schaffner: Everything depends on how broadly parents withhold their children from vaccination. Some parents are very selective, withholding only this or that vaccine; others withhold their children from all vaccines.
The broader the withholding, the more likely it is that one of these viruses will be reintroduced into the United States among susceptible persons.
As you know, we had a big polio scare in the suburbs of New York a few years ago, and we had one paralytic case in a young adult male who had never been vaccinated — and that poliovirus had been introduced from abroad.
So, these other illnesses that are contagious but not as contagious as measles will also be reintroduced into the United States.
Measles is at the forefront because it is the most contagious and easily transmitted. These others may take longer to appear in the United States because they are less contagious.
Schaffner: Reality has tempered my optimism recently. It will take time to reach out to all of these populations to provide them with information and reassurance that vaccination is in the best interest of not only those individual children or your children, but also your entire community.
There are increasingly more children, adolescents, and adults living among us who are immune suppressed, whether because of an illness or because they’re receiving immunosuppressive medication to treat an illness. These people cannot receive the measles vaccine because it’s a live, attenuated virus, and their immune system can’t fight off this virus.
We can protect them by having all the rest vaccinated and protected, making it very hard for the virus to get past us to them. We have a responsibility not only to our children but also to those who are more frail who live among us.
If you have any concerns, please talk to your doctor or your children’s doctor. They will be ready to talk with you about this and provide reassurance.
We have to do this at the local level and try to influence those individual communities to, over time, change people’s attitudes and feelings and make them more welcoming to vaccines. It’s a large task.